
Barrier Birth Control
and Non-Hormonal Devices
Barrier Birth Control and Non-Hormonal Devices
Barrier birth control is any physical barrier worn by the male or female partner that prevents the sperm either from entering the vagina or reaching the cervix. It is also the best form of birth control to prevent STDs (sexually transmitted diseases).
7 Types of Barrier Birth Control
7 Types of Barrier Birth Control
Male and Female Condoms
Male condoms
Also known just as condoms, are the most popular form of barrier birth control. They are over the counter, sold in pharmacies and most convenient stores, and are affordable and easy to use. The male partner will wear the condom, in this case to cover the penis, preventing sperm from going inside the vagina upon ejaculation. It is advised to wear the condom before any penetration occurs to ensure pre-ejaculatory fluid isn’t released into the vagina as this can cause pregnancy. When used perfectly, the male condom is proven 98% effective; however, in real-world use, condoms are about 87% effective. Condoms are intended for single use only- after ejaculation a new condom should be used. Do not reuse used condoms.
Female condoms
Thin, plastic pouches––are also available, and like a vaginal ring, are inserted into the vagina but contain no hormones. These condoms are to be removed each time after sex. They are proven 80% effective. If a female condom is broken during penetrative sex, then pregnancy may occur.
Condoms are the only form of birth control that help against STDs and are the safest backup contraception should any hormonal birth control become irregular.

Sponge
The sponge is another non-prescription birth control option. It is a small round piece of soft foam coated with spermicide that can be inserted up to 24 hours before sexual intercourse. You must run the sponge first under water to activate the spermicide before insertion. It is proven to be 88% effective and you are encouraged to leave it in after sex for at least six hours to avoid pregnancy, but not more than 30 hours to avoid infection. To remove the sponge, you simply pull on the loop attached to it.

Diaphragm
A dome-shaped device made of latex or silicone, the diaphragm needs to be individually fitted by a healthcare professional. It is prescription-based. Unlike the sponge, it does not come with spermicide. You will need to apply spermicidal gel onto the rim and in the dome before inserting into the vagina. The diaphragm is reusable but should be washed well and dried before putting it back in its case. It should also be checked regularly for wear or holes. Replace it after two years or have it refitted should you gain or lose ten pounds, have a baby, or have surgery around your abdomen or pelvis. One-sized diaphragms that fit most women are also available by prescription.

Cervical Cap
Like the diaphragm, a cervical cap is a small, dome-shaped device made of plastic that stays in place via suction. The cervical cap comes in three sizes. Your size will be determined by your healthcare professional. Spermicidal gel should be applied to the rim and dome. The cap should be checked (by pressing on the dome) before and after sex to ensure it is fully covering the cervix. A cervical cap can be put in several hours before having sex, and must be left in at least 6 hours after sex. Caps should not be left in longer than 24 hours after sex. The device should be replaced every year or before that should any damage occur, similar again to the diaphragm.

Spermicide
Except for the sponge, which already comes with spermicide, this contraceptive can be used with all types of birth control. It is a chemical that inactivates sperm before entering the uterus. It comes in four forms: foam, gels or creams, suppositories, or films (thin sheets inserted close to the cervix). Insert it into the vagina with the help of an applicator. Apply the spermicide 10 to 15 minutes before sex. It is only effective for one hour, meaning reinsertion will be necessary after each hour, or for every new act of sex.

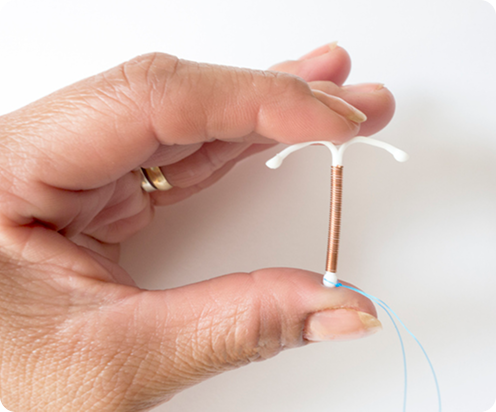
Copper IUD
A copper intrauterine device (IUD) is a small, T-shaped plastic device wrapped in copper that prevents pregnancy. It’s also known as a non-hormonal IUD. The copper IUD creates an inflammatory reaction in the uterus that’s toxic to sperm, while also changing the lining of the uterus and cervical mucus, making it less hospitable to sperm. It can serve as emergency contraception up to five days after sex, however, it does not prevent STDs. It may also cause heavier cramping and bleeding (period) for the first six months of use.
Contraceptive Gel (Phexxi)
While this is not the same as a spermicide, but is used in a similar way – Phexxi is a gel that is inserted into the vagina before sex and lowers the pH in the vagina, thereby reducing the chances of sperm cells from reaching an egg. Phexxi does require a prescription.
During a study, Phexxi was found to be 86% effective at preventing pregnancy, but another study suggests that when used perfectly (inserted immediately or up to one hour before sex – and must be used every time), it can be 93% effective. It should be mentioned that Phexxi can be used with other forms of birth control, including some hormonal methods, but cannot be used with a vaginal ring. A few reported side effects from contraceptive gel, include vaginal burning and discomfort, increased chance of yeast infections, and bacterial vaginosis. This method is not recommended for those who are prone to urinary tract infections.

What Are the Side Effects of Barrier Birth Control?

Typically, there aren’t any side effects of using barrier birth control as these methods are only used during the act of sex, unlike forms of hormonal birth control which are taken daily/continually . However, if it is your first time using a condom or a diaphragm, there may be some initial discomfort. A condom, made out of latex, usually doesn’t differ from the feel of a penis, but its texture can sometimes be rough or rigid. A diaphragm or cervical cap may also cause some discomfort in the vagina if it is not placed correctly. If it moves around during sex, this may cause more discomfort or worry. Should you feel uncomfortable using barrier forms of birth control, talk to your partner and explore other ways of preventing pregnancy.
Disclaimer:
When exploring birth control methods, it’s essential to research various options and consult a healthcare professional to make an informed decision that aligns with your unique needs and lifestyle. Each individual’s body and circumstances are different, so it’s important to choose a method that feels right for you—free from external pressures or influences. Remember, this is a personal choice that directly impacts your health and well-being. Prioritizing your comfort and understanding will empower you to make the best decision for your reproductive health.
What Are the Side Effects of Barrier Birth Control?
Typically, there aren’t any side effects of using barrier birth control as these methods are only used during the act of sex, unlike forms of hormonal birth control which are taken daily/continually . However, if it is your first time using a condom or a diaphragm, there may be some initial discomfort. A condom, made out of latex, usually doesn’t differ from the feel of a penis, but its texture can sometimes be rough or rigid. A diaphragm or cervical cap may also cause some discomfort in the vagina if it is not placed correctly. If it moves around during sex, this may cause more discomfort or worry. Should you feel uncomfortable using barrier forms of birth control, talk to your partner and explore other ways of preventing pregnancy.

Disclaimer:
When exploring birth control methods, it’s essential to research various options and consult a healthcare professional to make an informed decision that aligns with your unique needs and lifestyle. Each individual’s body and circumstances are different, so it’s important to choose a method that feels right for you—free from external pressures or influences. Remember, this is a personal choice that directly impacts your health and well-being. Prioritizing your comfort and understanding will empower you to make the best decision for your reproductive health.
Birth Control Resources
View moreFEMM Health
FEMM Health- Telemed
FEMM Health
Have Questions About Barrier Birth Control?
Ask Our Confidential Chatbot!








